Medical insurance credentialing can be a daunting task for healthcare providers in New Jersey. It is a necessary process that allows healthcare providers to participate in insurance networks and receive reimbursement for the services they provide. However, the process of medical insurance credentialing can be time-consuming and complex, and it can be challenging to navigate the requirements of different insurance companies.
In this blog, MSM Credentialing Services will discuss everything you need to know about medical insurance credentialing in New Jersey, including the requirements, process, and timeline. MSM Credentialing will also offer tips and advice to help you navigate this process successfully and avoid common pitfalls.
What is Medical Insurance Credentialing?
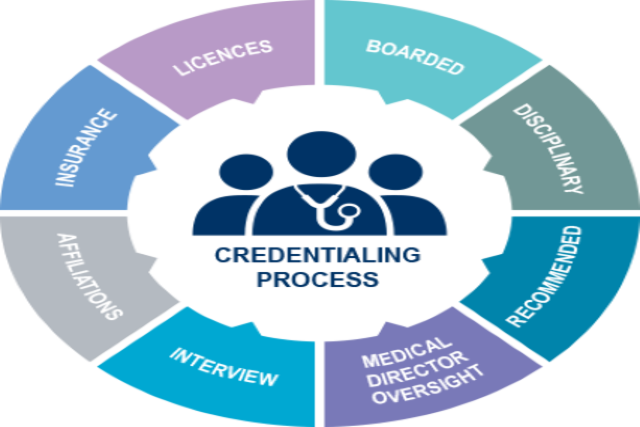
Medical insurance credentialing is the process of obtaining approval from insurance companies to participate in their provider networks. This process involves verifying the qualifications and credentials of healthcare providers, including education, training, licensure, and certification.
Medical insurance credentialing is necessary for healthcare providers who want to participate in insurance networks and receive reimbursement for their services. Participating in insurance networks allows healthcare providers to expand their patient base and increase their revenue streams.
Requirements for Medical Insurance Credentialing in NJ
The requirements for medical insurance credentialing in New Jersey vary depending on the insurance company. However, there are some general requirements that most insurance companies require healthcare providers to meet. These requirements include:
- Active licensure in the state of New Jersey
- Board certification or eligibility
- Malpractice insurance
- NPI number
- DEA registration (if applicable)
- Up-to-date CME credits
- Adherence to the insurance company’s policies and procedures
It is essential to note that the requirements for medical insurance credentialing can vary from one insurance company to another. Therefore, it is crucial to check with each insurance company you wish to participate in to ensure that you meet their specific requirements.
The Process of Medical Insurance Credentialing in New Jersey
The process of medical insurance credentialing in New Jersey can be time-consuming and complex. The following is a general overview of the steps involved in the process:
Step 1: Determine the insurance companies you want to participate in
Before you begin the credentialing process, you need to determine which insurance companies you want to participate in. You can research insurance companies online or contact them directly to obtain information about their credentialing requirements.
Step 2: Gather all necessary documents and information
Once you have identified the insurance companies you want to participate in, you need to gather all the necessary documents and information required for credentialing. This includes your medical license, board certification, malpractice insurance, NPI number, DEA registration (if applicable), and other documentation as required by the insurance company.
Step 3: Complete the credentialing application
After gathering all the necessary documents and information, you need to complete the credentialing application for each insurance company. The credentialing application will require you to provide information about your education, training, licensure, certification, and other relevant information.
Step 4: Submit the application
Once you have completed the credentialing application, you need to submit it to the insurance company for review. The insurance company will review your application and verify your credentials and qualifications.
Step 5: Follow up with the insurance company
After submitting your application, it is essential to follow up with the insurance company regularly to ensure that your application is being processed. You may also need to provide additional information or documentation if requested by the insurance company.
Step 6: Approval or denial
Finally, the insurance company will either approve or deny your application. If your application is approved, you will be added to the insurance company’s provider network and can begin providing services to patients covered by that insurance company. If your application is denied, you may need to address any deficiencies in your credentials or qualifications and reapply in the future.
Timeline for Medical Insurance Credentialing in New Jersey
The timeline for medical insurance credentialing in New Jersey can vary depending on the insurance company and the complexity of the application. Generally, the credentialing process can take anywhere from 60 to 120 days from the time you submit your application.
It is essential to keep in mind that the credentialing process can take longer if there are any deficiencies in your application or if the insurance company requires additional information or documentation.
Tips for Successful Medical Insurance Credentialing in New Jersey
Here are some tips to help you navigate the medical insurance credentialing process successfully in New Jersey:
Research the insurance companies: Before beginning the credentialing process, research the insurance companies you want to participate in. Make sure you understand their credentialing requirements and policies to avoid any surprises.
Keep accurate records: Keeping accurate records of your education, training, licensure, certification, and other relevant information can help expedite the credentialing process and avoid delays.
Be proactive: Follow up regularly with the insurance company to ensure that your application is being processed and address any deficiencies promptly.
Work with a credentialing service: Consider working with a credentialing service to help you navigate the credentialing process. Credentialing services can help you gather the necessary documentation, complete the application, and follow up with the insurance company.
Stay up-to-date with requirements: Keep up-to-date with changes to the credentialing requirements and policies of the insurance companies you participate in to avoid any compliance issues.
Outsourcing Medical Insurance Credentialing in New Jersey
Outsourcing medical insurance credentialing in New Jersey is an option that many healthcare providers consider to help them navigate the credentialing process. Working with a credentialing service can help you save time, reduce administrative burdens, and avoid common pitfalls.
When outsourcing medical insurance credentialing in New Jersey, it is essential to work with a reputable and experienced credentialing service. Look for a service that has a track record of success and can provide references from satisfied clients.
Conclusion
Medical insurance credentialing in New Jersey is a necessary process for healthcare providers who want to participate in insurance networks and receive reimbursement for their services. The credentialing process can be time-consuming and complex, but with proper planning and preparation, healthcare providers can navigate this process successfully.
Remember to research the insurance companies you want to participate in, gather all necessary documentation, complete the application accurately and promptly, follow up regularly with the insurance company, and keep up-to-date with changes to the credentialing requirements. At MSM Credentialing, we can help you successfully navigate the medical insurance credentialing process, so you can focus on providing quality care to your patients.